Case Studies
Healthcare Marketing in Action
At Corpuz Wilson Digital, we help companies transform complex communications into meaningful experiences. Here are examples of our work with leading regional insurers, showing how strategy, empathy, and execution come together to build trust, improve engagement, and deliver measurable results.

Case Study 1
Medicare Retention & Acquisition
Challenge:
Many Premera members had transitioned from employer coverage to individual plans. Upon
enrollment, they encountered frustrations: a confusing member site, delayed mailings, and a
lack of regular digital communications. The result was lower satisfaction and higher call volumes.
Our Work:
We developed an engagement plan to improve comprehension, accessibility, and satisfaction:
Website refresh: clearer navigation, glossary, and improved search.
Rewritten and redesigned materials: concise benefit guides and resources designed for readability.
Unified messaging: consistent tone across website, emails, digital, print, and call scripts.
Education videos: short explainers simplifying complex Medicare benefits.
Communication calendar: coordinated outreach across topics, benefits, and health reminders.
Regular member emails: highlighting new digital tools, plan education, and preventive care tips.
Results:
More members used digital tools instead of relying on mailed materials.
Satisfaction improved as communications became clear, consistent, and accessible.
Reduced member confusion and call center complaints through proactive outreach and education.
Positioned Premera as a more trusted partner in Medicare, aligning experience with expectations of today’s retirees.
Case Study 2
Prospect & Member Engagement
Challenge:
Blue Cross of Idaho needed new ways to connect with members across diverse product lines,
including Medicare,
government programs, small group plans, and large group plans. Traditional communication channels weren’t reaching
everyone effectively, and engagement goals demanded a digital-first approach.
Our Work:
Launched mobile program tailored for Medicare members and group segments.
Designed an email marketing strategy that provided consistent, relevant updates to government
program members and broker audiences.Crafted campaigns that adhered to strict CMS compliance while staying approachable and easy to understand.
Results:
50% of Blue Cross of Idaho Medicare members opted in to receive text messages,
a rate significantly above industry averages.SMS and email campaigns exceeded benchmarks for open and click-through performance,
ensuring timely delivery of critical healthcare information.Blue Cross of Idaho gained a scalable, compliant model for future digital outreach.
Case Study 3
Broker Communications
Challenge:
Blue Cross of Idaho needed to strengthen relationships with its broker community and reduce confusion
during critical enrollment periods.
Information gaps were leading to broker frustration.
During AEP (Annual Enrollment Period) and Open Enrollment, communication overload and unclear
updates caused unnecessary issues for brokers and internal teams.
Solution:
We launched a targeted email program for brokers, designed to be:
Frequent and timely during high-volume periods:
Increased email frequency October–December (AEP)
Continued through January (Open Enrollment)
Clear and actionable: Focused on updates, key dates, and resources brokers needed immediately.
Results:
65–70% open rates — far above industry benchmarks.
High click-through rates on key resources and updates.
Broker satisfaction increased, with fewer last-minute emergencies and clearer processes.
Internal teams saved time by resolving fewer avoidable issues.
Case Study 4
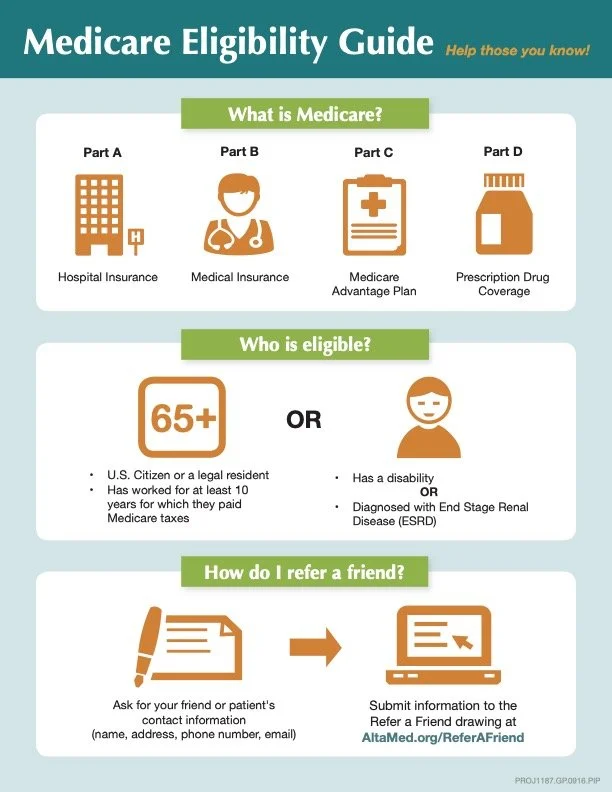
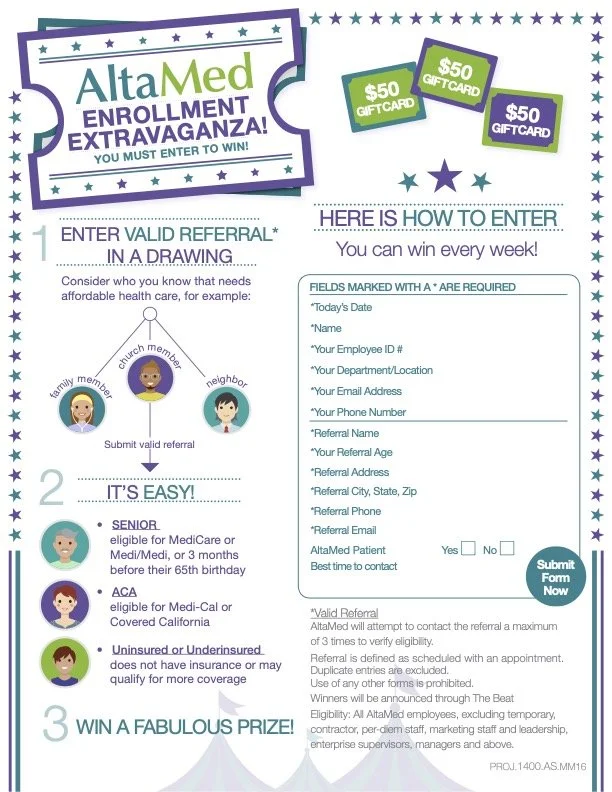
AltaMed Health Services
Engaging Medicare-Eligible Patients
Client:
AltaMed Health Services is a large network of clinics serving predominantly Hispanic neighborhoods
in South Los Angeles, with many patients eligible for Medicaid and Medicare.
Challenge:
AltaMed faced a significant gap:
Many patients were aging into Medicare eligibility but weren’t aware of Medicare Advantage
options.The organization needed a way to educate eligible patients and connect them with the right
resources at the right time.
Solution:
Developed a direct mail campaign targeting existing patients who were nearing Medicare eligibility.
Direct Mail List: Focused on existing patients, ensuring relevance and familiarity.
Multi-Touch Campaign:
An initial letter introduced Medicare Advantage options.
A birthday card mailing provided a personalized follow-up as patients approached eligibility.
Integrated Outreach: The call-to-action connected patients to AltaMed’s customer service department,
which also ran outbound call campaigns to schedule appointments.
applications directly.
Results
Higher engagement from patients approaching Medicare eligibility.
Streamlined appointment scheduling and increased broker-facilitated enrollments at clinic locations.
Strengthened patient trust by keeping all outreach within the familiar AltaMed ecosystem.
Turning Complexity Into Clarity
From SMS opt-ins to Medicare Advantage engagement plans, these case studies show how healthcare organizations can move beyond transactional communication to create trusted member relationships. At Corpuz Wilson Digital, we bridge the gap between compliance and connection, helping members feel informed, empowered, and cared for.